Understanding Wisdom Teeth: Why They Cause Trouble
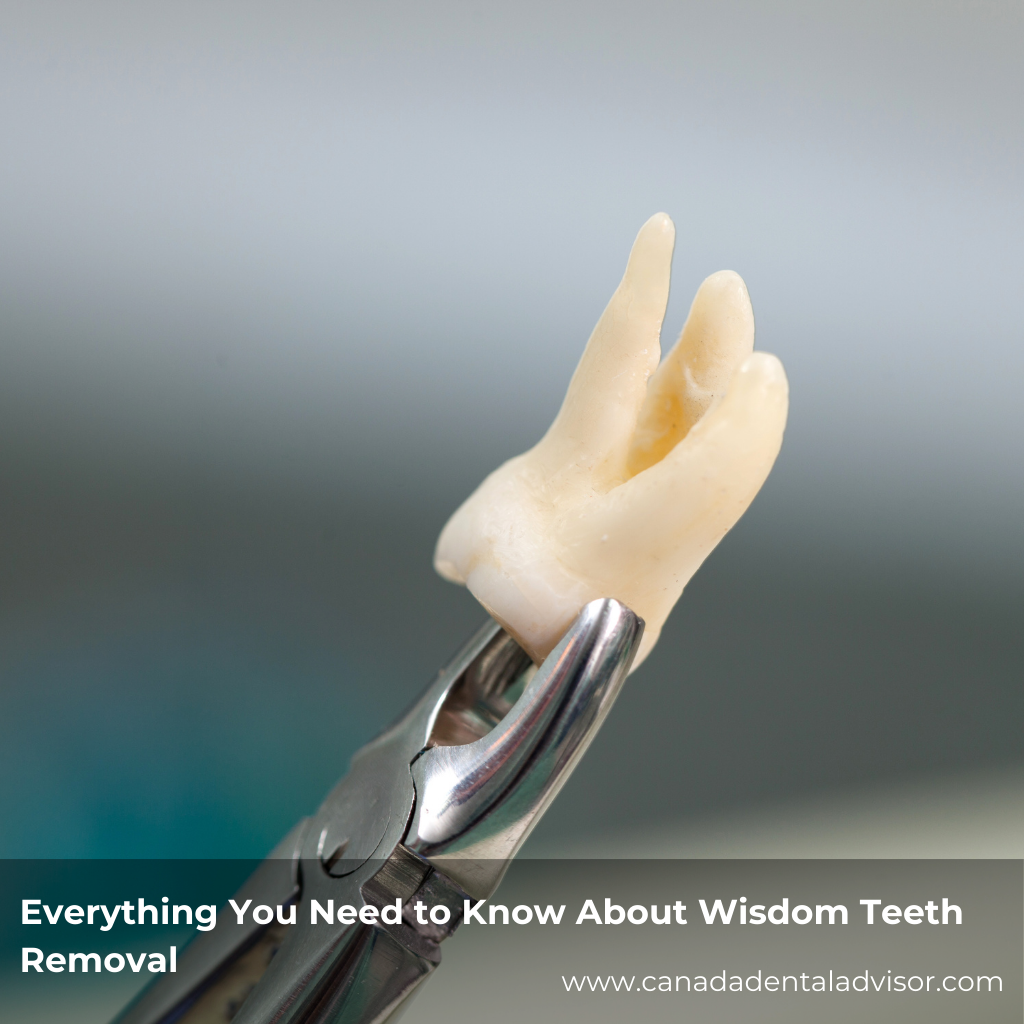
Wisdom teeth, or third molars, typically erupt between the ages of 17 and 25. While some people never develop them, many end up with four—one in each corner of the mouth. The problem? Our modern jaws are often too small to accommodate these extra molars.
Common issues include:
-
Impaction (teeth trapped beneath the gum line)
-
Infection or abscesses
-
Damage to nearby teeth
-
Crowding and misalignment
-
Cysts or tumors
And while some people have no symptoms at all, others experience sharp pain or swelling seemingly out of nowhere.
One Size Doesn’t Fit All: The Case for Individualized Care
Meet Sam and Alex—two very different patients.
Sam is a healthy 19-year-old with all four wisdom teeth impacted, but no pain yet. Alex is 35, a smoker, with one partially erupted wisdom tooth that’s infected.
If both received the same treatment plan, it could spell trouble.
Why Individualized Plans Matter:
-
Medical History and Risk Factors
-
Patients with heart conditions, diabetes, or bleeding disorders require special precautions.
-
Smokers and older adults face higher complication risks.
-
-
Type and Position of the Teeth
-
Fully erupted vs. partially impacted vs. horizontally impacted teeth require different surgical approaches.
-
-
Patient Comfort and Anxiety
-
Sedation options (local anesthesia, IV sedation, general anesthesia) should match patient needs and comfort levels.
-
-
Recovery Support and Lifestyle
-
A college student might bounce back in a few days. A parent juggling work and kids might need extended aftercare and planning.
-
How Individualized Care Enhances Treatment Outcomes
A personalized plan ensures that everything from pre-op prep to post-op healing is aligned with the patient’s needs. Here’s how that plays out in real life:
1. Faster, Safer Recovery
-
Tailored antibiotic regimens reduce infection risks.
-
Custom pain management plans reduce the need for narcotics, supporting safer healing.
2. Fewer Complications
-
Surgeons can avoid nerve damage or sinus complications by using advanced imaging (like 3D scans) to guide precise removal.
3. Proactive Preventive Care
-
Early intervention can prevent more complex surgeries later, especially in teens and young adults.
Better Compliance Begins with Trust
When patients feel heard and understood, they’re more likely to follow instructions—before and after surgery.
Examples of Improved Compliance:
-
Personalized instructions help patients remember what not to eat, how to rinse, and when to take medications.
-
Ongoing follow-up reduces the risk of dry socket, one of the most painful complications.
-
Customized reminders (texts or app-based) increase follow-through on checkups.
A one-on-one conversation that includes visuals, risk explanations, and realistic recovery timelines builds patient confidence—and that goes a long way in ensuring they stick to the plan.
Long-Term Oral Health: It Starts with Smart Planning
Wisdom teeth removal isn’t just about today’s pain—it’s about preserving the integrity of your smile in the years to come.
Long-Term Benefits of Individualized Planning:
-
Prevention of misalignment: Especially important for patients with orthodontic work.
-
Reduced bone loss: Gentle techniques minimize trauma to the jaw.
-
Ongoing health screening: Dentists can use this opportunity to assess gum health, bone density, and even detect early signs of other oral diseases.
Patients who receive personalized plans often feel more connected to their care journey—and this engagement leads to better oral hygiene habits, consistent dental visits, and more proactive prevention.
Conclusion: Your Smile Deserves a Tailored Approach
Whether you’re 18 or 38, wisdom teeth removal doesn’t have to be overwhelming. When your dental team crafts a treatment plan just for you, the experience becomes safer, smoother, and more empowering.
So if you’ve been told those molars need to come out, don’t settle for a cookie-cutter approach. Ask about individualized care—and take an active role in your journey to better oral health.
Your mouth is unique. Your treatment should be too.
FAQs About Wisdom Teeth Removal
1. At what age should I consider wisdom teeth removal?
Most people have their wisdom teeth evaluated in their late teens or early twenties, but adults can have them removed later if issues arise.
2. Is wisdom teeth removal always necessary?
Not always. If the teeth are healthy, fully erupted, and not causing problems, your dentist may recommend monitoring instead of extraction.
3. How long does it take to recover?
Typical recovery ranges from 3–7 days for most patients. An individualized plan can optimize healing and reduce discomfort.
4. What’s the difference between impacted and erupted wisdom teeth?
Erupted teeth have broken through the gum line. Impacted teeth remain beneath the gums and may grow at odd angles, requiring surgical removal.
5. Will I be awake during the procedure?
It depends on your chosen sedation method. Local anesthesia keeps you awake but pain-free, while IV or general sedation allows for a sleep-like experience.
6. Can wisdom teeth affect my other teeth?
Yes, especially if they’re impacted or growing at an angle. They can cause crowding, root damage, or shifting of nearby teeth.
7. What should I eat after surgery?
Stick to soft foods like yogurt, applesauce, and mashed potatoes for a few days. Avoid hot, spicy, or crunchy items.
8. What is dry socket, and how do I avoid it?
Dry socket occurs when the blood clot at the extraction site is dislodged. To prevent it, avoid straws, smoking, and vigorous rinsing for a few days post-op.










Leave a Reply