Why individualized care plans matter
Individualized care plans use patient-specific information—clinical findings, risk factors, lifestyle, socioeconomic context, and personal preferences—to create a realistic, targeted pathway for oral health. Compared with generic recommendations, individualized plans:
-
Focus resources where they’re needed most (high-risk sites, behavior change support).
-
Reduce unnecessary interventions and overtreatment.
-
Improve patient understanding and ownership of care.
Improved treatment outcomes: targeting biology and risk
The core of better outcomes is accurate risk stratification and targeted interventions.
Diagnose, stratify, intervene
-
Use risk assessments (caries risk, periodontal risk) to determine frequency and intensity of treatment.
-
Match interventions to risk: high-risk patients benefit from fluoride varnish, antimicrobials, or more frequent professional care; low-risk patients need reinforcement of basic prevention.
-
Incorporate technology: intraoral photos, charting, salivary tests, and real-time plaque indices can refine diagnosis and track progress.
Personalized home-care prescriptions
An individualized plan prescribes not just “brush twice daily” but specific tools, techniques, and schedules: electric toothbrush models with particular brush head types, interdental brushes sized for the patient’s embrasures, and tailored fluoride regimens. Matching tools to need improves plaque control and healing.
Enhanced patient compliance: making behavior change realistic
Compliance is rarely about willpower alone—plans that account for motivation, habits, and barriers perform better.
Co-create the plan
When clinicians collaborate with patients—setting shared goals, discussing tradeoffs, and choosing acceptable strategies—patients are far more likely to follow through. Co-creation increases buy-in and frames care as a partnership.
Use small, specific steps
Behavioral science favors micro-goals and habit stacking. For example:
-
Start with switching to a recommended electric toothbrush and a two-minute timer app.
-
Add interdental cleaning three nights a week, then daily once the habit is established.
Leverage technology for support
Electric toothbrushes with timers, pressure sensors, and smartphone apps can provide immediate feedback and gamified progress tracking. Reminders, progress reports, and clinician-viewable data (with consent) create accountability and let clinicians reinforce positive change in follow-ups.
Fostering long-term oral health: continuity and adaptation
Individualized plans are dynamic documents, not static prescriptions.
Regular reassessment
Schedule reassessments tied to risk: a high-risk patient may return every 3 months; a low-risk patient every 6–12 months. Each visit reassesses risk factors and adapts the plan—treatment intensifies or steps back depending on progress.
Address social determinants and access
Long-term success requires addressing barriers such as cost, transportation, or health literacy. An individualized plan might include referrals to community resources, selection of cost-effective tools, or translated instructions to ensure continued adherence.
Education plus reinforcement
Sustained oral health combines clear education (why a step matters) with reinforcement (positive feedback, simplifying routines). Provide written or digital takeaways customized to the patient’s needs and literacy level.
Practical example (brief)
Patient A: 58-year-old with localized periodontitis, heavy calculus, limited manual dexterity, and busy schedule.
Individualized plan:
-
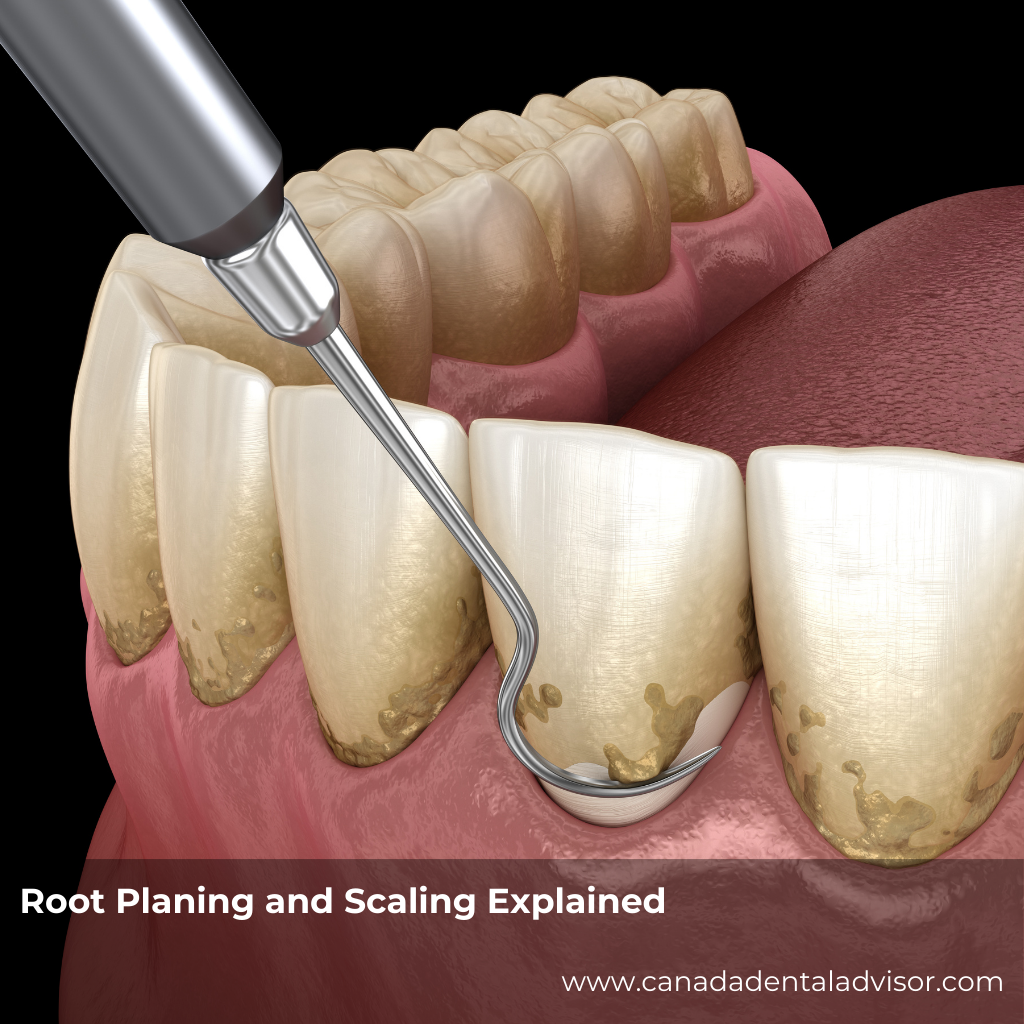
Immediate: scaling and root planing for affected areas, prescription antimicrobial rinse.
-
Home care: oscillating-rotating electric toothbrush with a compact head and pressure sensor; interdental brushes sized to embrasures; caregiver demonstration and accessible written instructions.
-
Follow-up: 6-week healing check, 3-month periodontal maintenance, remote app check-ins for brushing metrics.
Measuring success
Track objective and subjective outcomes:
-
Clinical: reduced pocket depths, lower plaque scores, fewer new caries.
-
Behavioral: frequency/duration of brushing (from app data), interdental cleaning reported.
-
Patient-reported: comfort, perceived ease, and satisfaction.
Conclusion & call to action
Individualized care plans bridge the gap between clinical best practices and real human lives. By aligning biologic risk, patient behavior, and practical tools—like the right electric toothbrush—clinicians can improve outcomes, boost compliance, and create sustainable oral health. Start small: introduce risk stratification at your next visit, co-create one personalized home-care step, and schedule a targeted follow-up. Over time, those small changes compound into big, lasting results.
FAQ (common questions)
1. What is an individualized care plan?
A customized, evidence-based strategy that matches preventive and therapeutic actions to a patient’s unique clinical risks, behaviors, and preferences.
2. How does an electric toothbrush fit into a personalized plan?
Electric toothbrushes can be matched by head size, motion type, and features (timers, pressure sensors) to address dexterity, plaque control needs, and motivation.
3. Will individualized plans increase chair time?
Initially, they may require slightly longer assessments, but targeted care reduces unnecessary procedures and follow-up interventions, saving time long-term.
4. How do clinicians measure patient compliance?
Through objective measures (plaque scores, app data from electric brushes) and patient self-reports, combined with clinical outcomes.
5. Are individualized plans cost-effective?
Yes—by focusing resources where they yield the most benefit (preventing disease progression), they often reduce expensive emergency treatments later.
6. How often should plans be reviewed?
Review frequency should match risk: high-risk every 3 months, moderate every 4–6 months, low-risk annually or biannually.