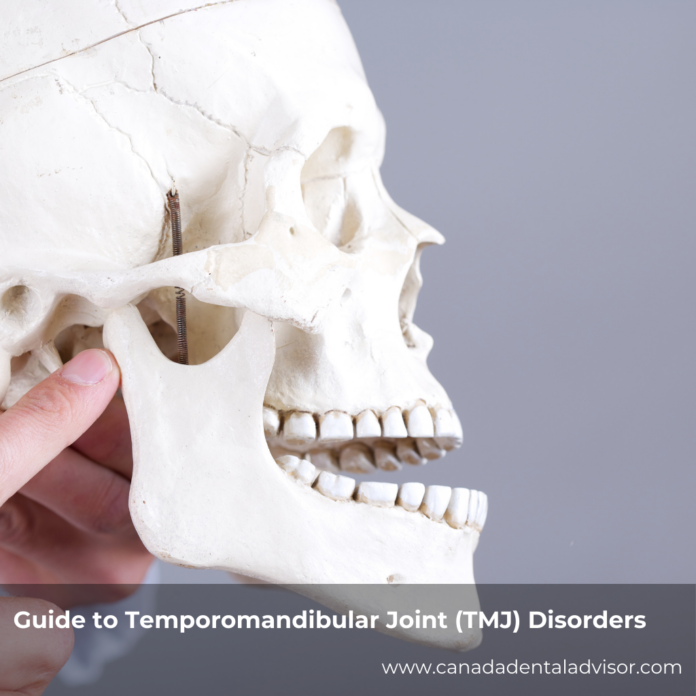
Personalized TMJ Disorder Treatment in Canada: A Practical Guide
Jaw pain that won’t quit. Clicking or popping when you open wide. Headaches that start near the ear. If this sounds familiar, you’re not alone. Many Canadians live with temporomandibular joint (TMJ) disorders. The good news: most people feel better with a plan that’s made just for them, not a one-size-fits-all fix.
What is the best treatment for TMJ disorder?
There isn’t one ‘best’ TMJ fix. The effective approach is a personalized plan after a thorough exam. Dentists combine a custom splint, jaw exercises, stress management, short-term medication, and follow-ups to adjust care, reduce pain, and protect long-term oral health.
Maria’s Story: Why personalization matters
Maria tried a generic nightguard from the pharmacy, pain relievers, and a few stretches she found online. Nothing lasted. When she finally saw a dentist who took time to assess her bite, muscles, posture, stress, and sleep, her plan changed. She received a custom splint, simple daily jaw exercises, and stress-coping tools. With regular check-ins and small adjustments, her pain eased and the clicking settled. Her story is common. Personalized care works because it targets your exact drivers—not someone else’s.
TMJ Disorders 101: Simple signs and common causes
TMJ disorders affect the joints that connect your lower jaw to your skull and the muscles around them. Symptoms can include jaw pain or tenderness, headaches, ear pain or fullness, clicking or popping, chewing trouble, and jaw locking (getting stuck open or closed). Symptoms can flare during busy or stressful times, then calm down.
What can trigger TMJ problems?
Everyone’s list is a bit different, but common causes include teeth grinding or clenching (often at night), stress and muscle tension, jaw or neck injury, arthritis, a misaligned bite, poor posture, and sometimes sleep-related issues. If grinding is part of your picture, learn about evidence-based solutions for teeth grinding to protect your teeth and joints.
“In most cases, discomfort from TMD can be managed with self-care and nonsurgical treatments.” — American Dental Association
Why one-size-fits-all fixes often fall short
Two people can have the same symptom—say jaw pain—but for different reasons. A basic nightguard may help one person but not another if the real issue is neck posture, daytime clenching, or an inflamed joint. Personalized plans focus on the root causes, which improves comfort and long-term results. When care is tailored to your life—your work hours, stress level, sleep, habits, and goals—you’re much more likely to stick with it.
What a personalized TMJ plan looks like
Think of your plan as a toolkit. Your dentist and care team choose the right tools for your situation and adjust them over time.
1) Comprehensive assessment
Your visit should include a careful history (pain patterns, triggers, past dental work, injuries), an exam of your jaw joints and muscles, bite analysis, and a check of posture and habits. Imaging (X-rays, panoramic, or CBCT) is used when needed to rule out other issues. This step is key—it guides everything that follows.
2) Customized appliance (occlusal splint)
A custom-made splint helps support the jaw and spread biting forces so your joints and muscles can rest. It’s designed from impressions or digital scans to fit your bite. Not all splints are the same. The design, material, and timing are chosen for you. If grinding is a concern, ask your dentist about custom night guards for bruxism and TMJ and how they differ from over-the-counter trays.
3) Physical therapy and gentle jaw exercises
Targeted stretches and strengthening can calm tight muscles and improve movement. Your provider may suggest tongue-to-palate rest position training, controlled opening, side-to-side glides, and simple posture resets. Small, frequent sessions (minutes per day) are often better than long, infrequent efforts.
4) Behavioural and stress care
Stress can fuel jaw clenching without you noticing. Practical strategies—like breath pacing, short walks, heat to relax sore muscles, and setting reminders to unclench during the day—can make a surprising difference. If anxiety at the dentist is a barrier, ask about comfort options and gradual desensitization.
5) Short-term medication, when appropriate
Some patients benefit from anti-inflammatories or a short course of muscle relaxants to settle a flare. Your dentist or physician will review your medical history and any interactions. Medication supports the plan; it doesn’t replace the other pieces.
6) Sleep and posture habits
Sleep quality and body position affect the jaw. Simple changes—like a supportive pillow, avoiding stomach sleeping, and taking short posture breaks if you work at a screen—reduce strain on the neck and jaw muscles. If snoring or possible sleep apnea is present, a medical sleep assessment may help.
7) Follow-ups and fine-tuning
TMJ care is rarely “set and forget.” Expect check-ins to fine-tune your splint, progress exercises, and adjust strategies based on what’s working. This is where long-term results happen.
When to seek care—and what to expect in Canada
Book a dental visit if you have ongoing jaw pain, frequent headaches near the temples, jaw locking, or chewing pain. In Canada, private dental insurance may cover parts of TMJ care (for example, splints or physical therapy), but details vary by plan. Provincial health plans rarely cover TMJ treatment for adults. Your dental team can provide estimates and help you plan care in stages if needed.
The dentist’s role: coach, partner, and monitor
TMJ disorder affects more than a joint—it touches sleep, stress, posture, and habits. A supportive dentist will listen, explain your options in plain language, and design a plan around your goals and routine. You should feel like a partner in the process. For a deeper primer on basics, see this complete overview of TMJ symptoms, diagnosis, and treatment.
Realistic timelines and results
Some people notice less pain and fewer clicks within weeks. For others—especially when symptoms have lasted a long time—it can take a few months. That’s normal. The goal is steady progress: fewer flares, easier chewing, better sleep, and protection against tooth wear and joint strain over time.
Simple daily routine: a starter plan
Use this as a conversation guide with your dentist—your actual plan may differ:
Morning
Gentle jaw range-of-motion (1–2 minutes), heat or warm shower to relax muscles, check posture before starting work, soft-food swaps if you’re sore.
Daytime
“Unclench” reminders every hour (tongue on the palate; lips closed, teeth apart), quick neck and shoulder stretch break, water bottle nearby (hydration helps muscles).
Evening
Custom splint/night guard as advised, brief stretch routine, light self-massage of tender jaw muscles, screen break before bed for better sleep.
Evidence-backed links and resources
Because grinding and clenching are common TMJ triggers, learning how to address them pays off. Explore practical strategies in evidence-based solutions for teeth grinding and talk with your dentist about whether a splint or other supports make sense for you.
Frequently asked questions
1) Do I need imaging for TMJ?
Not always. Many cases can be assessed with a history and exam. Your dentist may order X-rays or other imaging if your symptoms suggest joint changes, prior injury, or if treatment isn’t working as expected.
2) What’s the difference between a custom splint and a store-bought guard?
Custom appliances are made from your bite and adjusted over time. They’re designed to protect the joints and reduce muscle overload. Over-the-counter guards may help in the short term but can change your bite or feel uncomfortable, which hurts compliance.
3) Will I have to wear a splint forever?
Usually not. Many people wear a splint at night during a flare and taper as symptoms improve. Your dentist will guide timing based on your progress and risks (like grinding or heavy tooth wear).
4) Can stress alone cause TMJ pain?
Stress can lead to clenching and tense jaw muscles, which may trigger symptoms. That’s why stress tools—like scheduled “unclench” breaks and breath pacing—often make a real difference alongside your dental treatments.
5) What about surgery?
Surgery is rarely needed. Most people get relief with non-surgical care: a custom splint, exercises, stress care, and targeted short-term medication. If your dentist suspects significant joint damage, they’ll discuss next steps and refer you if needed.
6) How long until I feel better?
Some feel improvement in a few weeks; others need a few months. The key is sticking with your plan and attending follow-ups so your dentist can adjust care. Small gains add up.
Conclusion
TMJ disorders can be frustrating, but you’re not stuck. A personalized plan—built from a careful assessment and tuned to your life—can quiet pain, reduce clicks, protect your teeth and joints, and support better sleep. Ask your dentist about a custom roadmap that includes a well-fitted splint, exercises, stress tools, and regular check-ins. If grinding plays a role, integrating the right appliance matters. Learn how custom night guards for bruxism and TMJ fit into long-term protection. With the right plan and a supportive team, lasting relief is realistic—and so is confidence in your smile and bite.