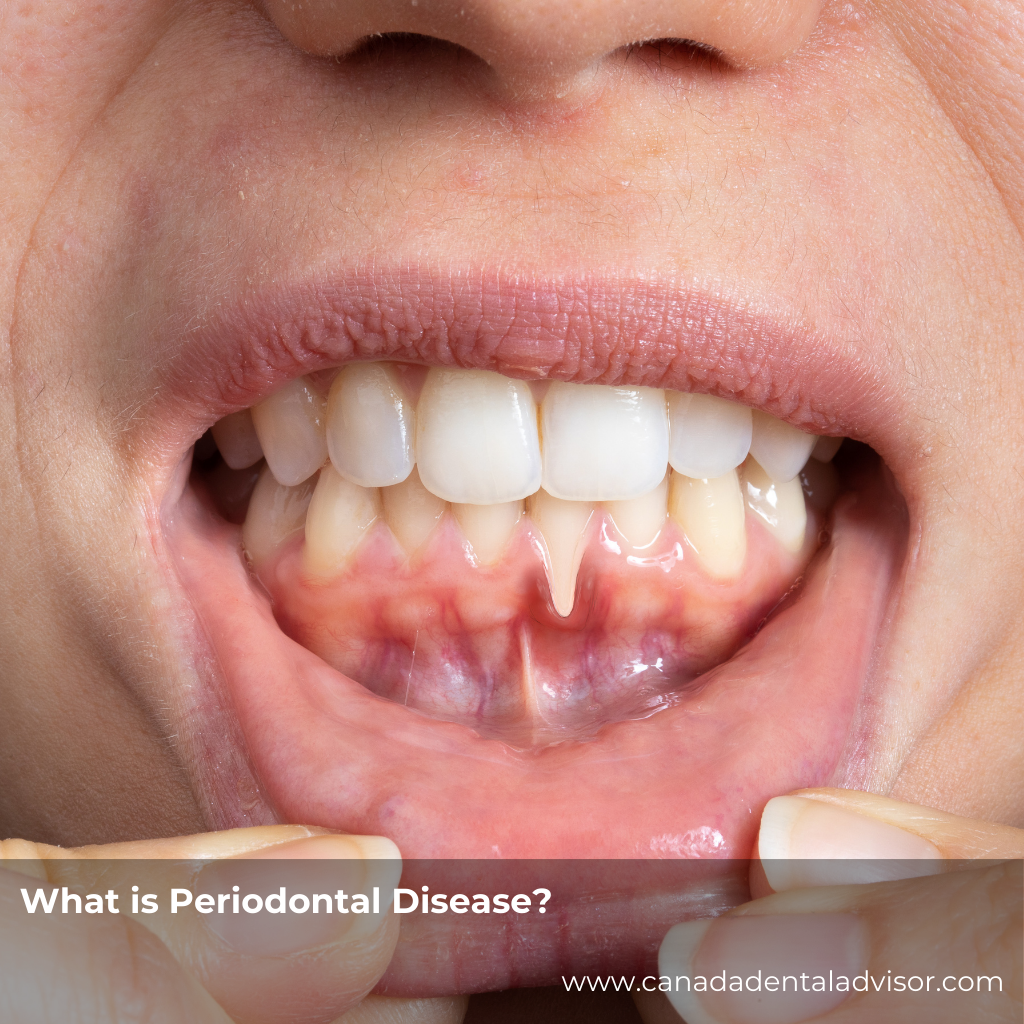
Understanding Periodontal Disease
Periodontal disease is a chronic infection of the gums and supporting bone that hold teeth in place. It typically begins with gingivitis—red, swollen, and bleeding gums caused by plaque buildup. If left untreated, it can advance to periodontitis, where the gums pull away from the teeth, creating pockets that harbor bacteria and lead to bone loss.
Key signs and symptoms include:
-
Persistent bad breath
-
Gums that bleed easily
-
Gum recession or teeth appearing “longer”
-
Loose or shifting teeth
-
Tender or swollen gums
Without proper care, periodontal disease can result in tooth loss and even affect systemic health, linking to conditions like heart disease and diabetes.
Why Individualized Care Matters
No two patients experience periodontal disease in the same way. Factors such as genetics, medical history, lifestyle habits, and oral hygiene routines all influence how the disease progresses and how treatment should be approached.
An individualized care plan considers these variables, ensuring that treatment isn’t a “one-size-fits-all” approach. Instead, it provides patients with strategies tailored to their unique needs, making care more effective and sustainable.
How Individualized Care Improves Treatment Outcomes
1. Targeted Therapies for Better Results
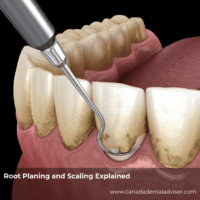
Standard treatments like scaling and root planing (deep cleaning) are often effective, but some patients may need additional therapies such as:
-
Antibiotics or antimicrobial rinses to control infection
-
Laser therapy for less invasive pocket cleaning
-
Surgical options for advanced disease
By tailoring treatment, dentists can maximize healing and minimize unnecessary procedures.
2. Addressing Risk Factors
An individualized plan looks beyond the gums. For example:
-
A diabetic patient may need closer monitoring due to slower healing.
-
Smokers may require more frequent cleanings.
-
Patients with a family history of periodontal disease may benefit from preventive therapies earlier.
By addressing these factors, treatment becomes proactive instead of reactive.
Enhancing Patient Compliance Through Personalization
1. Clear, Relevant Education
When patients understand why specific recommendations apply to their situation, they’re more likely to follow through. A young adult might respond to reminders about protecting their smile, while an older patient may care more about keeping natural teeth for life.
2. Simplified Home Care Routines
Some patients thrive with electric toothbrushes and interdental brushes, while others prefer water flossers. Tailoring home care instructions increases the chance that patients will actually adopt these habits.
3. Building Trust and Motivation
When patients feel their dentist is listening to their concerns and creating a plan “just for them,” they’re more motivated to stay consistent. Personalized care fosters trust, which directly improves compliance.
Fostering Long-Term Oral Health
1. Regular Maintenance
Periodontal disease is chronic, which means it requires ongoing care. Individualized recall schedules (every 3–4 months instead of 6 for some patients) ensure early detection of relapse.
2. Whole-Body Wellness Connections
Because gum disease is linked to systemic health, care plans can be coordinated with physicians for conditions like diabetes or cardiovascular disease. This holistic approach helps patients view oral health as part of overall wellness.
3. Empowering Patients for the Future
Personalized care isn’t just about today’s treatment—it’s about equipping patients with the tools and confidence to protect their oral health for decades.
Conclusion
Periodontal disease can be silent and destructive, but it doesn’t have to steal your smile. With individualized care plans, patients receive treatment that matches their unique needs, improving outcomes, boosting compliance, and building habits that support lifelong oral health.
If you’re concerned about gum health or want to know more about personalized treatment options, schedule a visit with your dentist today. Prevention and early action are the keys to a healthier, stronger smile.
Frequently Asked Questions
1. What is the main cause of periodontal disease?
Plaque buildup from poor oral hygiene is the primary cause, though factors like genetics, smoking, and medical conditions also play a role.
2. Can periodontal disease be cured?
While advanced disease cannot be fully reversed, it can be effectively managed with proper treatment and maintenance.
3. How often should I see my dentist if I have periodontal disease?
Most patients benefit from visits every 3–4 months for professional cleanings and monitoring.
4. Does gum disease affect overall health?
Yes. Research shows links between periodontal disease and conditions such as heart disease, diabetes, and even pregnancy complications.
5. What treatments are available for periodontal disease?
Options range from non-surgical scaling and root planing to antibiotics, laser therapy, and surgery, depending on severity.
6. Is gum recession permanent?
Recession can’t always be reversed naturally, but surgical procedures like grafts may restore gum tissue in some cases.
7. What’s the difference between gingivitis and periodontitis?
Gingivitis is the early stage, with inflamed gums. Periodontitis is the advanced stage, involving bone loss and deeper gum pockets.
8. Can I prevent periodontal disease?
Yes—daily brushing, flossing, professional cleanings, and personalized preventive care can greatly reduce your risk.






Leave a Reply